Optimal or Delayed Cord Clamping, what is it and should you be choosing it for your baby?
Cutting the cord! For some birth partner’s it’s a rite of passage, for other’s they’d rather hand it over to the midwife! We’ve often thought about WHO’s going to ‘cut the cord’, but have you given any consideration as to WHEN they’re going to cut it?
After your baby has been born, it will still be attached to the placenta, by the umbilical cord. The placenta is still providing oxygenated blood to the baby until it has stopped pulsating (approximate 3-5 minutes after birth). After that, the placenta will detach from the uterus and be born.
Did you know? There’s usually no need to cut the cord before it has stopped pulsating, or even before you have birthed the placenta.
Early cord clamping became commonplace in the sixties following the introduction of new drugs in an attempt to prevent too much maternal bleeding after birth. Thought this was never based on any evidence!
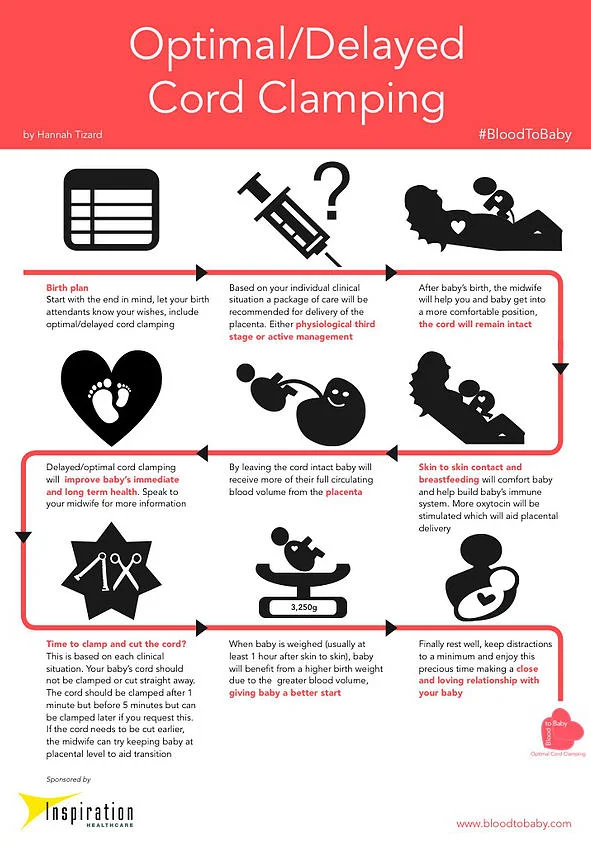
Following more recent research, The World Health Organisation now recommends waiting until the cord has stopped pulsating before cutting, usually between 3-5 minutes. But why? I’ve summarised the evidence into bitesize chunks, which will hopefully help you make your decision.
A Summary of the Evidence
What are the benefits?
Baby continues to receive oxygenated blood until breathing is established and this has been shown to reduce the chances of any breathing difficulties (particularly in preterm infants).
Around 1/3 of the baby’s blood remains in the placenta at birth. Allowing this to transfuse into e baby where it belongs, can lower the risk of anaemia or compromised heart function.
Optimal Cord Clamping reduces the risk of late onset sepsis and the need for a blood transfusion in preterm babies.
There is a reduced chance of Mum having a retained placenta (where the cervix closes before the placenta has been born).
But, what are the Risks?
A small study has shown a slightly increased risk of baby developing jaundice following delayed cord clamping, though usually physiological (normal) and most experts agree that the benefits outweigh the risks in this case.
Current guidance in the UK recommends OCC for all births, unless there is a medical reason to cut the cord sooner. If you are planning an ‘active third stage’, where your placenta is helped out through an injection of synthetic oxytocin, you can still have OCC, but they recommend the cord is cut before 5 minutes.
Though it is written into the guidelines, it’s still worth putting into your own birth plan if it’s important to you.
As with any choice you make around pregnancy and birth- gather the information, weight up the risks and the benefits and make a decision that feels right for you and your baby!
References:
1. Hutchon DJR. Immediate or early cord clamping vs delayed clamping. Journal of Obstetrics and Gynaecology, November 2012; 32: 724-729
2. Mercer JS, Erickson-Owens DA; Rethinking placental transfusion and cord clamping issues. J Perinat Neonat Nurs. 2012; 26; 3; 202-217.
3. Van Rheenen P. Delayed cord clamping and improved infant outcomes. BMJ. 2011; 343:d7127
4. Pan American Health Organization. Beyond survival: Integrated delivery care practices for long-term maternal and infant nutrition, health and development. World Health Organization. 2007.
5. Andersson O et al Effect of delayed versus early umbilical cord clamping on neonatal outcomes and iron status at 4 months: a randomised controlled trial. BMJ. 2011;343:d7157
6. Farrar D, et al. Measuring placental transfusion for term births: weighing babies with cord intact. BJOG. 2011; 118:70–75.
7. Wiberg N, Källén K, Olofsson P. Delayed umbilical cord clamping at birth has effects on arterial and venous blood gases and lactate concentrations. BJOG. 2008; 115: 697–703.
8. Rabe H, Reynolds G, Diaz-Rossello J. Early versus delayed umbilical cord clamping in preterm infants. Cochrane Database of Systematic Reviews.2004, Issue 4. Art. No.: CD003248. DOI: 10.1002/14651858. CD003248.pub2.
9. Mercer JS, et al. Seven-month developmental outcomes of very low birth weight infants enrolled in a randomized controlled trial of delayed versus immediate cord clamping. J Perinatology. 2010; 30; 11-16.
10. Richmond S, Wyllie J. European Resuscitation Council guidelines for resuscitation 2010. Resuscitation 81; 2010; 1389-1399.
11. Royal College of Obstetricians and Gynaecologists, UK. Clamping of the umbilical cord and placental transfusion. 2009. Scientific Advisory Committee Opinion Paper 14.
12. World Health Organisation. Guidelines on basic newborn resuscitation 2012. ISBN 978 92 4 150369 3.
13. Ceriani Cernadas JM, et al. The effect of early and delayed umbilical cord clamping on ferritin levels in term infants at six months of life: a randomized, controlled trial. Arch Argent Pediatr. 2010; 108(3); 201-208.
Megan Rossiter is a KG Hypnobirthing Teacher, Student Midwife and Mum. Positively Birthing Antenatal and Hypnobirthing Group and Private Classes are offered throughout Surrey in areas including Esher, Cobham, East Molesey, West Molesey, Thames Ditton, Surbiton, Thames Ditton, Chessington, Epsom, Ewell, Oxshott, Byfleet, Teddington, Hampton Hill, Hampton, Twickenham, Hampton Wick, Kingston and Beyond.